Tools and Strategies to Try
- Do 1 TIPP ✅ 2024-04-23
- Temp change
- Intense Exercise on Yoga via YouTube
- Paced Breathing
- Progressive Music Relaxation
- Do 1 sitting with stuck or intrusive thought: ✅ 2024-04-23
- Repeat the intrusive thought in my head for a few minutes with eyes closed
- Draw or write out the intrustive thought on iPad for 10 mins make it fun
- Sing a song about it
Key Findings
- Several family studies have found a substantially greater prevalence of OCD (∼10-fold increase) in the first-degree relatives of probands, compared with relatives of controls.1 2 3 4 The risk increases if the relative developed OCD as a child or teen. 5
- If you, your parent, or a sibling have OCD, there’s a 25% or one in four chance that another immediate family member will also have OCD. 6
- Population-based twin studies estimate the heritability of dimensional measures of obsessive–compulsive symptoms (OCS) to be 40–50%.7 8 9 10 11
- OCD can start in childhood or early adulthood. Most people who will have the disorder develop it by around age 25. 12
- People with OCD have some biological traits in common. These include hyperactivity in specific of the brain and an imbalance in neurotransmitters. 12
- Trials have shown that children and adolescents with OCD should begin treatment with the combination of CBT with a selective serotonin reuptake inhibitor or CBT alone, rather than only an SSRI. 13 14 15
- About 1 in 100 adults have OCD. 16
- Experts now believe OCD is caused by the brain and nervous system and not by family problems or behaviors learned in childhood. Genes may play a role in OCD. 16
- Prevailing theories indicate that OCD is a biological disease. Functional brain imaging studies have produced a model for pathophysiology of OCD which involves hyperactivity in certain subcortical and cortical regions. 17
- Childhood neurodevelopmental, behavioral, personality and environmental risk factors were associated with a diagnosis of OCD. 18
- DN likely gene disrupting and predicted damaging missense variants are enriched in OCD probands (RR 1.52, p=0.0005) and contribute to risk. We identified two high-confidence risk genes, each containing two DN damaging variants in unrelated probands: CHD8 and SCUBE1. 19
- A great study on OCD diagnosis, comorbities, and treatment approaches 20
Graphics and Visuals
Other Research
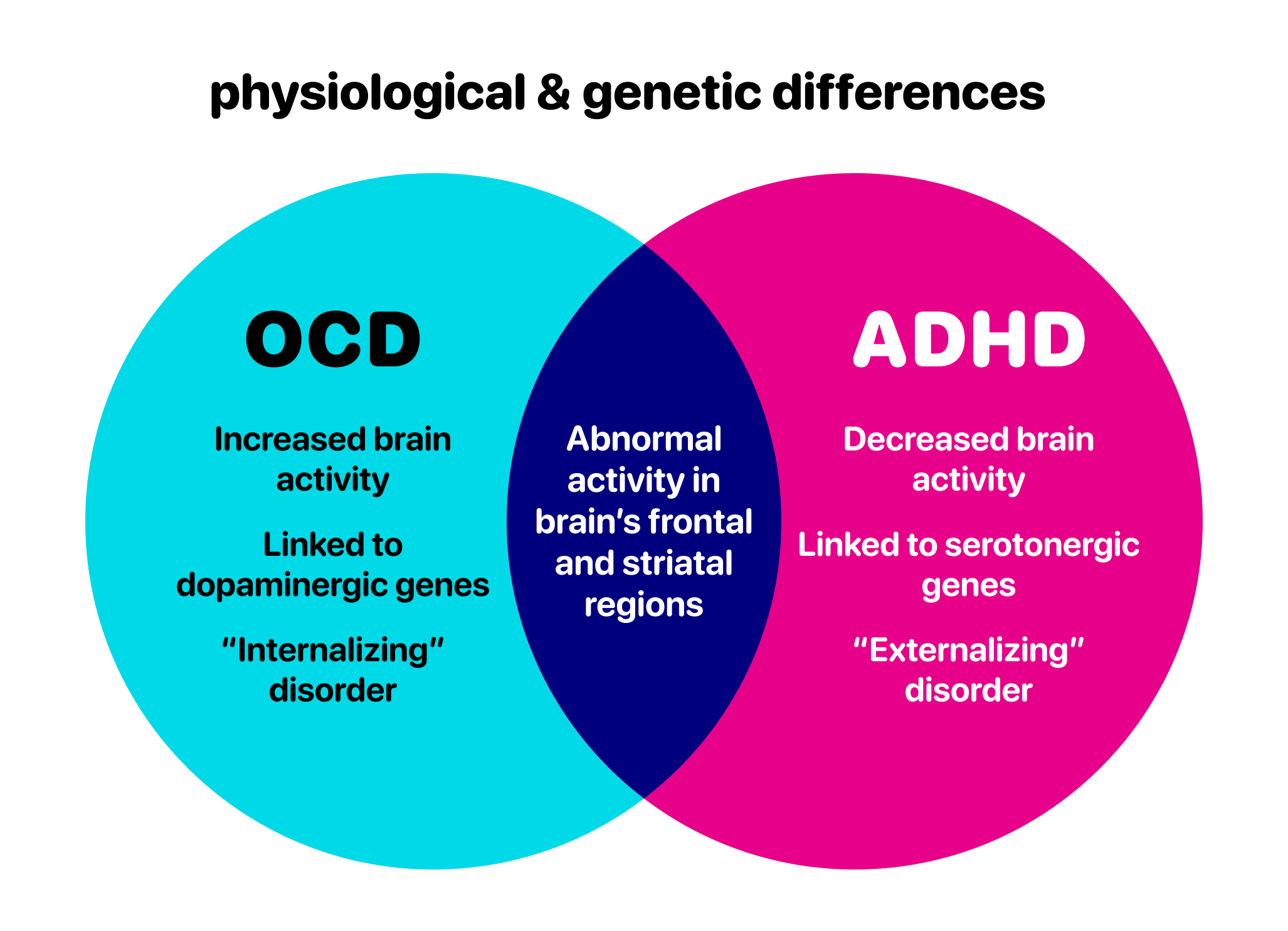
- Psychiatry Newsletter - Tourrette’s, OCD, ADHD: Closer Than We Thought
- When OCD and ADHD Coexist: Symptom Presentation, Diagnosis, and Treatment
Footnotes
Footnotes
-
Pauls DL, Alsobrook JP 2nd, Goodman W, Rasmussen S, Leckman JF. A family study of obsessive-compulsive disorder. Am J Psychiatry 1995; 152: 76–84. ↩
-
Nestadt G, Samuels J, Riddle M, Bienvenu OJ 3rd, Liang KY, LaBuda M et al. A family study of obsessive-compulsive disorder. Arch Gen Psychiatry 2000; 57: 358–363. ↩
-
Grabe HJ, Ruhrmann S, Ettelt S, Buhtz F, Hochrein A, Schulze-Rauschenbach S et al. Familiality of obsessive-compulsive disorder in nonclinical and clinical subjects. Am J Psychiatry 2006; 163: 1986–1992. ↩
-
Fyer AJ, Lipsitz JD, Mannuzza S, Aronowitz B, Chapman TF. A direct interview family study of obsessive-compulsive disorder. I. Psychol Med 2005; 35: 1611–1621. ↩
-
https://my.clevelandclinic.org/health/diseases/9490-ocd-obsessive-compulsive-disorder ↩
-
Clifford CA, Murray RM, Fulker DW. Genetic and environmental influences on obsessional traits and symptoms. Psychol Med 1984; 14: 791–800 ↩
-
Jonnal AH, Gardner CO, Prescott CA, Kendler KS. Obsessive and compulsive symptoms in a general population sample of female twins. Am J Med Genet 2000; 96: 791–796. ↩
-
Eley TC, Bolton D, O’Connor TG, Perrin S, Smith P, Plomin R. A twin study of anxiety-related behaviours in pre-school children. J Child Psychol Psychiatry 2003; 44: 945–960. ↩
-
Hudziak JJ, Van Beijsterveldt CE, Althoff RR, Stanger C, Rettew DC, Nelson EC et al. Genetic and environmental contributions to the Child Behavior Checklist Obsessive-Compulsive Scale: a cross-cultural twin study. Arch Gen Psychiatry 2004; 61: 608–616. ↩
-
Taylor S.. Etiology of obsessions and compulsions: a meta-analysis and narrative review of twin studies. Clin Psychol Rev 2011; 31: 1361–1372 ↩
-
https://www.massgeneralbrigham.org/en/about/newsroom/articles/obsessive-compulsive-disorder ↩ ↩2
-
Pediatric OCD Treatment Study (POTS) Team (27 October 2004). “Cognitive-Behavior Therapy, Sertraline, and Their Combination for Children and Adolescents With Obsessive-Compulsive Disorder: The Pediatric OCD Treatment Study (POTS) Randomized Controlled Trial”. JAMA. 292 (16): 1969–1976. doi:10.1001/jama.292.16.1969. PMID 15507582. ↩
-
Geller, Daniel A.; Biederman, Joseph; Stewart, S. Evelyn; Mullin, Benjamin; Martin, Andrés; Spencer, Thomas; Faraone, Stephen V. (November 2003). “Which SSRI? A Meta-Analysis of Pharmacotherapy Trials in Pediatric Obsessive-Compulsive Disorder”. American Journal of Psychiatry. 160 (11): 1919–1928. doi:10.1176/appi.ajp.160.11.1919. PMID 14594734. S2CID 8711232. ↩
-
Geller, Daniel A.; March, John (January 2012). “Practice Parameter for the Assessment and Treatment of Children and Adolescents With Obsessive-Compulsive Disorder”. Journal of the American Academy of Child & Adolescent Psychiatry. 51 (1): 98–113. doi:10.1016/j.jaac.2011.09.019. PMID 22176943. ↩
-
https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=1&contentid=633 ↩ ↩2
-
https://escholarship.org/content/qt9q45k5r8/qt9q45k5r8.pdf?t=rvnflu ↩
-
https://assets.cureus.com/uploads/review_article/pdf/200641/20231117-4512-6urkzg.pdf ↩